Is Early Diagnosis Important with Diabetic Eye Disease?
Are you a diabetic? Having diabetes can affect you in many ways, but you may not realize that having high blood sugar levels can even affect your eyes!
Diabetes happens when your blood sugar or blood glucose levels are higher than necessary.
People who have diabetes have a higher likelihood of developing several types of eye conditions.
Keep reading to learn more about diabetic eye disease and whether early detection affects treatment!
Macular Degeneration
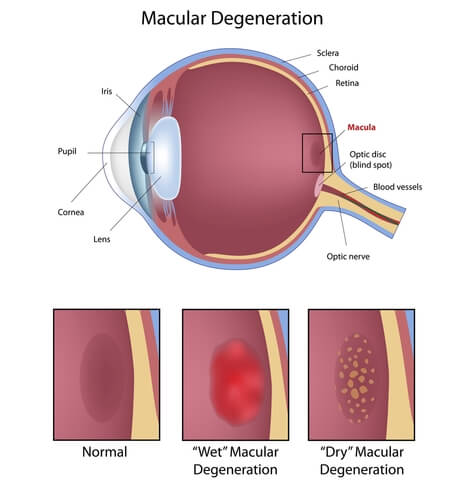
Age-related macular degeneration (AMD) is an eye condition that occurs when there’s damage to the macula, which is part of the retina. With macular degeneration, patients lose their central vision, making it impossible to see fine details. There are two kinds of macular degeneration: dry and wet.
Dry AMD
Of the two kinds of macular degeneration, dry AMD is the more common one. Dry macular degeneration occurs when parts of the macula get thinner due to aging. When this happens, clumps of a protein called drusen will develop.
Wet AMD
With wet AMD, it’s much less common than dry AMD. This form of macular degeneration forms when new, abnormal blood vessels begin to form under the retina. These abnormal vessels are weak and may leak fluid and blood, causing scarring on the macula.
Untreated or mismanaged diabetes can cause blood vessel changes. The best way to prevent vision loss from macular degeneration is to detect the condition early. Eye doctors may diagnose macular degeneration during a regular eye exam.
Your eye doctor will apply eye drops that dilate your pupils to inspect the macula for signs of damage. They will also use an ophthalmoscope. This device is a mirror that reflects light into the eye to examine the macula and retina.
If your eye doctor is aware of your diabetes and suspects macular degeneration, they may perform a fluorescein angiography. During fluorescein angiography, they’ll inject dye into your blood and take photos of the circulation in your eye. You may have macular degeneration if the dye leaks out of the blood vessels.
Glaucoma
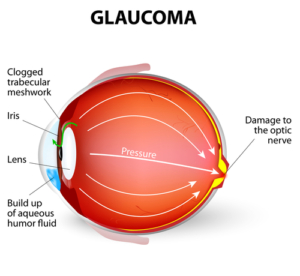
People with diabetes have twice the risk of developing glaucoma as people that don’t have diabetes. Diabetics may have the neovascular form of glaucoma.
Neovascular glaucoma occurs when blood vessels grow on the iris. The vessels block the flow of fluid out of the eye and increase intraocular pressure. Laser surgery can limit blood vessels in the iris and on the surface of the retina.
The best way to be prepared and avoid vision loss from glaucoma is to schedule regular eye exams with your eye doctor. In addition, those with diabetes may need twice-yearly exams to ensure early diagnosis of conditions like glaucoma.
To diagnose this condition, your eye doctor will use a technique called tonometry. Tonometry involves measuring intraocular pressure levels. High pressure from prolonged glaucoma may damage the optic nerve, causing irreversible vision loss.
Diabetic Retinopathy
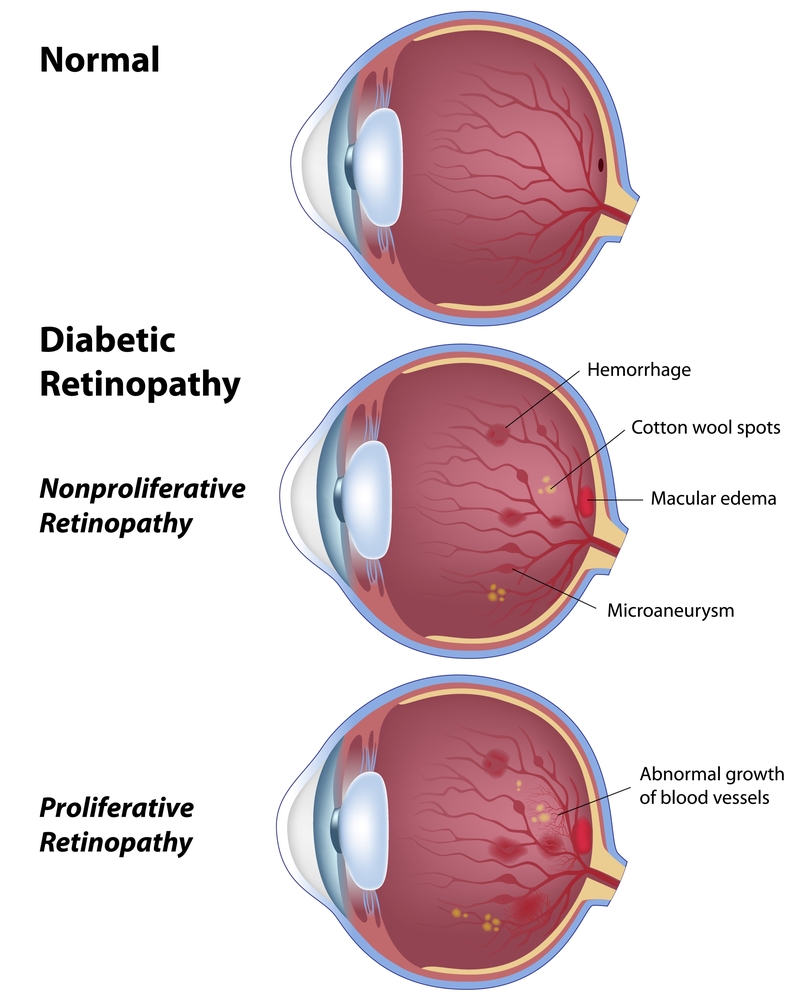
The most common diabetic eye disease is diabetic retinopathy. Diabetic retinopathy occurs when abnormal blood sugar levels cause damage to blood vessels in the eye. When this damage occurs, blood vessels around the retina bulge or start to leak.
Nonproliferative diabetic retinopathy
In the early stage of diabetic retinopathy, called nonproliferative diabetic retinopathy, you may not notice any symptoms. However, the blood vessels are weak, and the bulging blood vessels may leak fluid into the retina. If leaking occurs, it can lead to swelling of the macula.
Proliferative diabetic retinopathy
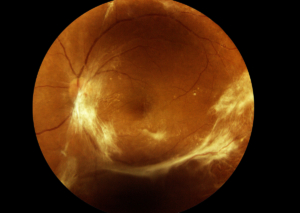
As diabetic retinopathy becomes more advanced, it moves into proliferative diabetic retinopathy. In this stage, new and more fragile blood vessels begin to form on the retina and move into the vitreous.
The vitreous is the gel-like fluid that fills the back of the eye. These new vessels may leak blood into the vitreous, making it more difficult to see. Patients may also experience a retinal detachment or the development of glaucoma.
Worsening damage can prevent light from entering the retina and make your vision blurry. Your brain can’t process what you see if the light doesn’t reach the back of the eye. You may see black spots where the vessels are leaking.
Your eye doctor will check for diabetic retinopathy by dilating your pupils during an eye exam. Then, they’ll use eye drops to increase your pupils’ size and look at the retina.
Early diabetic retinopathy may not need treatment. Your eye doctor may recommend more frequent eye exams to assess disease progression. You might be able to slow symptoms by managing your diabetes with the help of an endocrinologist.
Diabetic Macular Edema
If you have diabetic retinopathy, you may develop diabetic macular edema (DME). Diabetic macular edema occurs when broken blood vessels in the eye increase pressure.
Having consistently high blood sugar can lead to the damage of blood vessels in the eye. DME can happen at any stage of diabetic retinopathy.
You may have diabetic macular edema if your vision is doubled or blurry. Seeing floaters is also common. DME can cause blindness if it’s left untreated.
Ask your eye doctor about dilating your pupils to check for diabetic macular edema. This process helps your eye doctor assess both your retina and macula health.
Cataracts
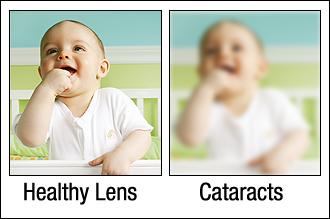
Although cataracts are part of the aging process, if you have diabetes, you’re more likely to develop cataracts. Cataracts are one of the most common causes of issues with sight for people with diabetes.
Common cataract symptoms include spotty and blurred vision. Some people notice halos around lights. Others say the world appears yellow or cloudy.
You may develop cataracts if your blood sugar levels are too high. The glucose can leak into the aqueous humor. This clear fluid fills the front of the eye between the lens and the cornea. It is 99.9 percent water and 0.1 percent nutrients, like vitamins, proteins, and sugars.
This mix of fluids supports corneal health and helps keep intraocular pressure levels balanced. Blood vessels damaged by diabetes can release too much sugar into the fluid, leading to increased eye pressure.
If you have diabetes, you should schedule a dilated eye exam every year. If you have other eye conditions, ask your eye doctor how often you should come in for appointments to keep your eyes as healthy as possible.
Do you have concerns when it comes to diabetic eye diseases? Request an appointment at Eye Consultants of North Dakota in Fargo, ND, to learn how our talented eye doctors can help!



